As we learn more about Complex Trauma (C-PTSD), it becomes increasingly clear that family scapegoating abuse (FSA) can lead to the development of C-PTSD symptoms, which are often misdiagnosed and mislabelled by Mental Health professionals if and when the FSA adult survivor seeks therapeutic treatment and support.
Defining Psychological Trauma
When you think of the word ‘trauma’, I would guess that many associations and images come to mind. Some might imagine that trauma has nothing to do with them due to the fact they did not experience a particular event that could be considered traumatizing. Therefore, it is critical that we understand trauma from the standpoint of experts who acknowledge the reality of C-PTSD.
As a practitioner who is also certified in Trauma-Informed approaches appropriate for psychotherapy and coaching, I prefer the definition of psychological trauma offered by Karen Saakvitne, which is as follows:
‘Psychological trauma is the unique individual experience of an event or of enduring conditions in which the individual’s ability to integrate his or her emotional experience is overwhelmed (i.e., his or her ability to stay present, understand what is happening, integrate the feelings, and make sense of the experience), or the individual experiences (subjectively) a threat to life, bodily integrity, or sanity’ (Pearlman & Saakvitne, 1995, p. 60).
In Saakvitne’s definition, trauma is an event or series of events that are experienced as being threatening to one’s life or sanity, leaving a person feeling so overwhelmed that they feel unable to cope. During such events (which can be repeated and chronic), the cognitive function of the brain may switch off, resulting in dissociation, which some may describe as “numbing out” or feeling “distant” or “disconnected” from events as they are occurring and also after.
As a result of this dissociative process, there is difficulty integrating these highly stressful, traumatic events into one’s experience, which can result in psychological ‘splitting’. For example, thoughts may be disconnected from feelings / emotions, or the intellectual understanding may be cut off from one’s bodily / sensory experience. Trauma is therefore associated with this lack of integration of one’s total experience of an event or series of events.
This might show up later in therapy as an inability on the traumatized client’s part to think about their stressful experiences in a coherent manner, and they may struggle to identify their experiences and feelings about all that has occurred. The traumatic events may be ‘split off’ from one’s everyday life experiences where they are ‘forgotten’ or seemingly discarded from one’s mind. In extreme cases, the client may even present with clinical signs of amnesia.
Psychological Trauma and Family Scapegoating Abuse (FSA)
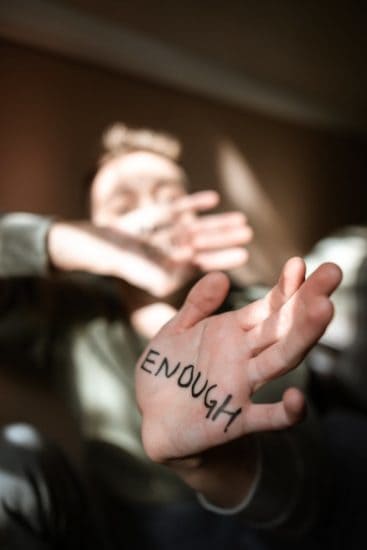
When you are in the ‘identified patient’ or ‘scapegoat’ role in your family-of-origin, you are experiencing trauma (including betrayal trauma and attachment trauma) that is repeated and uniquely psychologically destructive and overwhelming. You may have subconsciously employed many different ways to cope with the traumatizing effects of your home environment growing up or as an adult, including dissociating, disconnecting, or minimizing or rationalizing the covert or overtly abusive behaviors directed toward you by family members.
My research on FSA revealed that the experience of dissociation and ‘depersonalization’ is common to adult survivors of family scapegoating abuse, who often report feeling disconnected from events or from the reality of their situation as a target of FSA. In cases where a client does express strong feelings and emotions at the outset of their treatment with me, the primary feeling experienced is toxic shame (as discussed in my book on FSA, Rejected, Shamed, and Blamed) and a sense of abject humiliation, coupled by the idea that there must be something wrong with them for their family to treat them in the manner they do.
This is why many adult survivors of FSA struggle to acknowledge what has actually happened to them in their family-of-origin, as not only do they wonder if they are imagining how bad their family situation is; they also wonder if they are at fault and the cause of their own maltreatment within the family.
Another important point to be aware of is that because complex trauma is stored as emotional and bodily memories, there can be a conscious or subconscious expectation that the future will mirror the past, resulting in the experience of tremendous anxiety and trepidation when contemplating family contact (including family reunions and holiday gatherings) that others (including Mental Health professionals) may see as being irrational or fueled by paranoia.
Unaware that they are in fact trauma survivors, the adult survivor of FSA may also somaticize their psychological distress, resulting in various bodily aches and pains; depression; anxiety; or maladaptive coping behaviors such as abusing substances, including alcohol abuse and overeating. All this makes the FSA adult survivor extremely vulnerable when attempting to seek help for their psycho-emotional distress, as they will often be misdiagnosed with a variety of Mental Health issues, including Borderline (or Histrionic) Personality Disorder.
To learn more about family scapegoating abuse and its association with complex trauma, read my article, When Your Family Invalidates Your Experience of Abuse and Complex Trauma.
Do you identify with any of the points in this article? I’d love to hear from you in the comments, below. If you feel this article could help others, consider sharing it by scrolling down to the social media icons below my profile.
Hi Rebecca,
I looked up your book and I am going to pick it up in a few days. Funny I decided to search ptsd and scapegoat and this is where I landed.
I went NC with NMom 16 years ago. Didnt know anything about any of this at that time though. Recently had a visit from my GC brother and his new wife, and I became some kind of spaz when they were here. asking questions twice, not hearing the answers, talking fast, just completely not me. at all.
I was physically shaking when they were on the way and huge pit in the stomach when they arrived. It was aweful. I have not had to interact with him in 6 years and have talked to him 4 times in the last 10.
So I started to look for anyone else who might literally have a physical reaction to their golden child’s presence. Just presence. No bad words or tones, just casual visit. Last 2 phone calls from GC were about how its my duty to bla bla bla call my mother. I told him no both times. I will not.
So I am going to pick up the book and give it a read.
Pretty much as long as I dont see them. Any of them. Life is good. And I really cant do the phone with them either.
Thanks for the write up. Great Read.
Glad you picked up my book – You may relate to the chapters in their on complex trauma, based on your comment. Linking you to a list of resources I put together for FSA adult survivors; link to my YouTube channel is also there; I’m releasing a new video tomorrow: https://www.scapegoatrecovery.com/updated-fsa-recovery-resources-2023/
Hi Rebecca,
Many thanks for your helpful feedback with the necessary qualifications. I think my therapist is on the right track with the focus being on recovery from toxic shame due to trauma through reintegration of those split off parts. I currently live in southern Africa and am keen to for some kind of support group. Do you perhaps know of one for scapegoat survivors online? I know that Jay Reid (from SFO) has a FB support group, but you have to purchase his course for $500 before gaining entry. I have otherwise found his YouTube videos on scapegoat abuse to be very helpful.
I plan on purchasing those books you mention.
Hi Simon, one of my blog subscribers has a facebook group you can check out – Link: https://www.facebook.com/groups/1513500492048702/
Hi Rebecca,
Thank you for your insightful post. I plan to read more of them in the future. I am also interested in your book…
What caught my attention in particular is the BPD misdiagnosis. While my psychotherapist (who I think is good) has not diagnosed me with any personality disorder, I worry that I am either BPD or NPD or both. I worry about the former because of my tendencies to split and ruminate. These tendencies have become exacerbated by re-traumatization in recent years through narcissistic abuse, including at the hands of my scapegoating father. It would seem from what I have read by you and elsewhere that both splitting and rumination can be the result of CPTSD? Can the same also be said for object constancy?
I worry about an NPD diagnosis because of I see some parallels between my scapegoating father’s grandiosity and my own. As I understand, splitting is also a classic trait of NPD.
I have always considered myself to be an empathic co-dependent. The realisation of my toxic family of origin has only come to head in the past two years and I am in my mid-40s. I am my father’s scapegoat to this day and also recovering from being a surrogate spouse to my mother (when I still lived at home). Such was the narcissistic/ codependent (alcoholic/ enabler) dance that I experienced and forms the basis for my trauma history.
Integral to my recovery now (two years into therapy and currently at x2 per week) is shadow work, which can be very uncomfortable, but super helpful for reintegrating my shameful split off parts.
Good to hear from you, Simon. I think you would find my book (Rejected…) very helpful and I encourage you to get it; the Kindle version is currently on sale. Although I cannot offer you a formal professional opinion as you are not my client, I know of no person with NPD who could ever write a comment such as yours here. I would guess that you are suffering from complex trauma, and yes, splitting is typical, as is issues with object constancy, which can manifest as attachment trauma (have you and your therapist explored attachment trauma yet?) You might want to also pick up Janina Fisher’s workbook, ‘Transforming the Living Legacy of Trauma’. It is something you could work on with your therapist, and would likely help you both to know if C-PTSD is your primary issue. Shadow work can also be helpful; in complex trauma work, we would call this working with various ‘parts’ – which are often parts of the self that split off due to traumatic events or chronically stressful, frightening, unpredictable environments (the typical environment for a scapegoated child / adult child). You can find both Janina’s book and mine in my online shop here on my website. Link here: https://www.scapegoatrecovery.com/shop/
Thank you for your enlightening article. I’m 71, an American living in Italy and diagnosed with CPTSD as well as a dissociative disorder. I recently became aware that what had happened to me as a child was a direct result of being the family scapegoat. No one ever told me this but now it all makes sense. Both my parents were the abusers of my horrific childhood. I am fortunate that I have a good psychiatrist however I don’t think this is a topic that has been brought up specifically – family scapegoat). I will however discuss this as soon as I see her at my next session.
Hi Elle, I’m glad that you were able to make this connection and that you find my work on FSA (family scapegoating abuse) helpful. I’ve heard from many clinicians – including Psychiatrists – that they have appreciated my book and gained much from reading it; perhaps your Psychiatrist would be willing to take a look at my work, which is in part research-based from my days serving as Core Faculty at a Psychology grad school. This might then open up deeper discussions in your work with her, including going over the included FSA Assessment. Wishing you the very best!
Rebecca, you are so good with organizing your ideas into phrases that make appropriate/logical sense. My son found you and your writings with which we both identify! My recently deceased husband had us all under his spell as we tried to please him – just never well enough. My three adult children try to have nothing to do with either my son or me; they seem narcissistic; both of us feel we’re empathic. Son is in such physical – as well as emotional pain; and I have not been able to find a successful way to get him to go to any doctor or therapist. Anger, fear, and depression engulf him so that he no longer trusts me. I don’t know where to turn for some help for us.
Such a difficult situation! Your best recourse at this time might be to initiate your own therapy with a therapist trained in trauma-informed approaches and family systems. They can then guide you from there in regard to how you might best assist your son. You can screen for therapists in your area using the filters available on the therapist search tool available on https://psychologytoday.com.
Another excellent article which really resonates with me. I would love to order your book, but I can not and will not shop at Amazon. Is there some other way to order a copy?
Hi Star, you can order the eBook from any of these other online vendors: https://books2read.com/intro2fsa
Best, Rebecca
So very true. I was trained literally from birth to deny, suppress, and accept emotional, verbal, and occasional physical abuse. For years I just thought my (narcissistic) mother was crazy, my (golden child) older sister was spoiled, and my (enabling) father was weak. I was in my 50s before I realized that they had all effectively teamed up to abuse and denigrate me my entire life, making me, conveniently, the “crazy” one.
Even therapists failed to recognize or understand my role as the scapegoat. Despite my academic, professional, and personal successes, I have always struggled with emotional overeating, anxiety, and depression. But I managed to appear to “have it all together” (except for my weight), because I learned early on to NEVER show vulnerability. However, I always felt, deep down, that I was inherently flawed and unlovable.
Reading your book and learning online about scapegoating finally gave me the necessary pieces of the puzzle to fully understand the sick emotional dynamics that shaped my life. My parents are now dead, and my 2 sisters ganged up to exclude me from my share of the family inheritance, and even from our mother’s funeral. I have been No Contact now for about a year. It’s very freeing to stop walking on eggshells and stop seeking love from people who irrationally hate me. I was just diagnosed with serious cancer, and I realize how much having loving sisters would mean to me; but I have never had loving sisters. It’s just a fact. I don’t feel sorry for myself; I feel sorry for them.
Hi Calista, sounds like you have moved into that space of ‘radical acceptance’ I refer to in my book. I’m glad to hear that the puzzle is now more fully completed and you took the appropriate, necessary steps to prioritize your own well-being, free of all forms of abuse, while maintaining a compassionate, self-aware stance. May this continue to serve you well as you move toward a brighter future – which I hope will include becoming cancer-free!
Well done for getting your awareness and becoming strong enough to survive with deep insight into your situation. My experience was almost identical, including the two sisters and the inheritance. I didn’t get the eating issue but smoked weed instead (stopped long ago). Haven’t got cancer thankfully. I hope you get cured and go on to lead a fulfilling life. I personally do a bit of self development work daily via reading relevant material from professionals such as Rebecca and also meditate 2x 20 mins daily which is a great help. There is a lot of depth to this subject so we can continue to learn which helps release the trauma. I also took 5 years of therapy which was a great help also. Best of luck, strength and clarity to you.
Calista’s story sounds so similar to mine, including the two siblings—although for me one was a brother—who stood by without compassion towards me as my mother disinherited me before she died in 2019. I always felt like I was inherently defective. I was the firstborn and my mother coldly “joked” that I was the test one that needed to be tossed out, like the first pancake that was messed up on the griddle before the rest of the stack was successfully cooked. I took that to heart. I tried with all my might to be a good girl, but I always failed somehow.
I blamed myself for being imperfect and was the only member of my family to ever go to therapy. In 2008 I went in for yet-another round and convinced my counselor that I had Type-two Bipolar Disorder. However, none of the series of medications I was prescribed over the next few years was ever effective and when he brought up my relationship with my parents I assured him that there was nothing to see there. Eventually a divorce and limiting contact with my family-of-origin proved to be the medicine I truly needed.
I am now in group therapy where my role as the identified patient is being addressed and I am finding power in owning that I have, indeed, been the family scapegoat and that my husband had continued the pattern established by my mother. At age sixty-six, I am beginning to heal in ways I never knew I would.
I am wishing for Calista to find nurturing friends to be like siblings to her as she faces the challenges of cancer. I know what that particular longing for a sister is like. Hugs to you, Calista.